Hi, I'm Bryan
I got slow and squishy by my mid 40's. After a health scare, I got fit — and I discovered the outdoors.
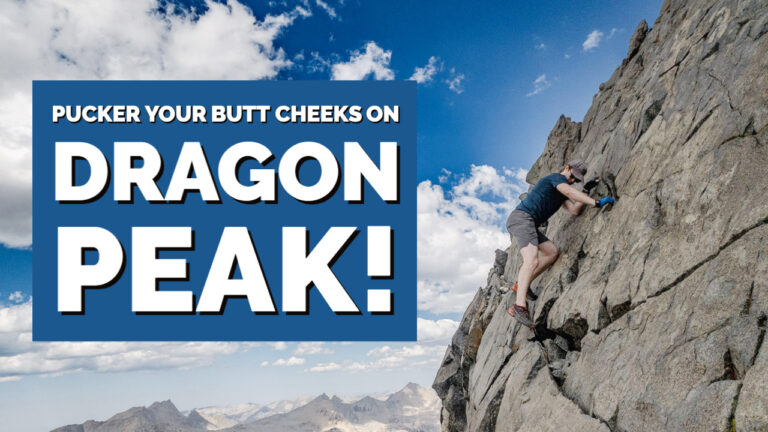
I fell in love with the beauty and awe one can only experience in wild places – especially in the High Sierras. What I thought was a midlife crisis ended up becoming a midlife renaissance. You can read more about my wanderings in the wilderness in my Adventure Journal or my Photo Gallery. Vocationally, I lead NCF California, where my team and I help generous families discover their family missions and build strategies for philanthropy. I hope my blog encourages you to get fit and live a life of joy and intention. Enjoy!